Children’s National Research Institute Academic Annual report 2019-2020

Center for Translational Research
Gift of $5.7 Million Connects Care and Research for Better Outcomes in Polycystic Kidney Disease
The marriage of caring for diseases and conducting research into understanding and creating improved treatments for those conditions drives progress.
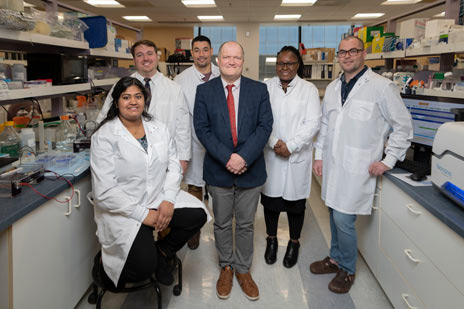
A $5.7 million gift received by the Center for Translational Research’s director, Lisa Guay-Woodford, M.D., will reinforce close collaboration between research and clinical care to improve the care and treatment of children with polycystic kidney disease (PKD) and other inherited renal disorders.
Dr. Guay-Woodford, the Elizabeth McGehee Joyce Professor of Pediatrics at Children’s National, is a world-renowned clinician and researcher in the field of inherited renal disorders, particularly PKD. After experiencing her care for their child with PKD and then hearing her speak about integrating clinical care and research for the condition, a family reached out to her about finding ways they could support both.
We developed a multipart plan that seeks to advance multiple aspects of PKD treatment in children. This includes improving clinical care, increasing new knowledge through research and disseminating that knowledge in ways that both families and providers can understand and use."
“What they were interested in was not just what is being done right now but also what kinds of things are on the horizon for PKD, especially for children,” said Dr. Guay-Woodford, “so we developed a multipart plan that seeks to advance multiple aspects of PKD treatment in children. This includes improving clinical care, increasing new knowledge through research and disseminating that knowledge in ways that both families and providers can understand and use.”
The philanthropic support funds several programmatic pillars aimed at progressing our understanding of these diseases from both clinical and research perspectives and at reinforcing the back-and-forth conversation between laboratory science and medical care. Highlights include:
- Providing coordinated care for children and families affected by renal cystic disease. The Inherited and Polycystic Kidney Disease program, launched in September 2019, provides access to a wide range of specialists so that “in a single, one-stop visit, we can address the myriad concerns they have, from nutritional through psychological and everything in between,” explains Dr. Guay-Woodford.
Strengthening global databases to capture PKD variations. The team will expand its outreach to other centers around the world — including Australia, Europe, India and Latin America — caring for patients with both the recessive and dominant forms of PKD to better understand the variety of ways the disease can manifest in children.
“We really don’t know a lot about kids with this disease; we mainly draw from the adult literature,” shepoints out. “How hard should we push to control a child’s blood pressure, knowing that could paradoxically hurt the kidneys? What are the issues involved in acute pain compared with chronic pain? How much do these pain flare-ups interfere with daily life and a child’s sense of self?”
- Filling a “desperate need” for biomarkers. Developing clinical trials for new therapies requires biomarkers for the disease course, which are instrumental in personalizing care for patients who may also have many additional chronic conditions. To date, these biomarkers have been elusive, but the funding underwrites pilot studies that will identify and validate these necessary markers.
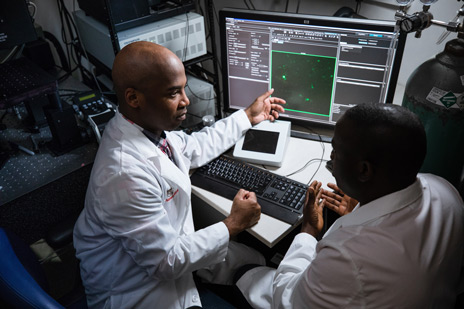
- Identifying genetic mechanisms that trigger kidney disease. About 500,000 people in the United States have PKD. In many cases, children inherit a genetic mutation, but often their mutation develops spontaneously. The fourth pillar of the PKD program provides funding for Dr. Guay-Woodford’s lab to continue research efforts that improve the mechanistic understanding of PKD.
The program’s crosscutting design forms an infrastructure that Dr. Guay-Woodford hopes will serve as a model for advancing knowledge in childhood diseases by bridging the clinical and research spectrum, with the engagement of philanthropic support from families.
“It’s the power of the art and science of medicine,” Dr. Guay-Woodford concluded. “They come to see people like me because of the science. If we can convey to patients and families that who they are and their unique concerns are really important to researchers, that becomes a powerful connection,” she says. “The art plus the science equals hope. That is what these families are looking for.”